Fungal acne can be difficult to distinguish and often misunderstood. So to shed some helpful insight on the subject, we have our panelists of Picky Experts here to discuss! Including dermatology specialist, Baokim, and dermatologists Dr. Mara and Dr. Jenny!
Misconceptions around fungal acne
Google search for “fungal acne” has skyrocketed over the past few years. A new buzz word in the beauty world, and everyone thinks they have it. Many people think they have fungal acne when they can’t find a solution to their acne, but that shouldn’t be your go-to skin diagnosis. Acne and fungal acne are different and we’re here to tell you why!
Question #1
What are the main major differences between acne and “fungal acne”?
 Baokim: I veer away from calling it ‘fungal acne’ since it’s not actually acne. The medical term for it is pityrosporum folliculitis or malassezia folliculitis, named after the yeast that causes the condition. Malassezia is actually part of our normal skin flora, but it can travel down the hair follicle, overgrow and create inflammatory papules and pustule. It’s not an infection. And with acne, the causes are multifactorial, but associated with bacteria (cutibacterium acnes).
Baokim: I veer away from calling it ‘fungal acne’ since it’s not actually acne. The medical term for it is pityrosporum folliculitis or malassezia folliculitis, named after the yeast that causes the condition. Malassezia is actually part of our normal skin flora, but it can travel down the hair follicle, overgrow and create inflammatory papules and pustule. It’s not an infection. And with acne, the causes are multifactorial, but associated with bacteria (cutibacterium acnes).
 Jenny: Malassezia folliculitis AKA fungal acne, is NOT acne. Acne is defined as a disease of the sebaceous glands with comedones present. Malassezia folliculitis is from the overgrowth of the malassezia yeast and like to live in sebum rich areas. It also belongs to the family of yeast that causes dandruff and tinea versicolor.
Jenny: Malassezia folliculitis AKA fungal acne, is NOT acne. Acne is defined as a disease of the sebaceous glands with comedones present. Malassezia folliculitis is from the overgrowth of the malassezia yeast and like to live in sebum rich areas. It also belongs to the family of yeast that causes dandruff and tinea versicolor.
 Mara: Malassezia folliculitis and acne are not the same, and here is how to tell the difference.
Mara: Malassezia folliculitis and acne are not the same, and here is how to tell the difference.
| Acne | “Fungal Acne” | |
| Causes | Chronic “inflammatory” disorder of hair follicles and sebaceous glands. Usually caused by over active sebum glands, inflammation, bacteria causing acne, etc. | A yeast that is a normal part of the skin’s flora, but an overgrowth can be due to inflammation of hair follicles. |
| Presentation | Open and closed comedones, red bumps, bumps with pus, sometimes nodules or cysts. | 1-2 mm papules and postules normally where the hair follicles are |
| Location | Face, chest, shoulders, back | Face, check, shoulders, back, back of arms and parts of the body where clothes rest |
Question #2
Is there any specific group that are more prone to developing such a condition?

 Baokim: It’s not that common. But those individuals with oily skin and sweat a lot are more susceptible since body oils and sweat make the perfect breeding ground. Also those that live in warmer or humid climates have increased risk. Immunocompromised and those on certain medications (like steroids or oral antibiotics) are also predisposed.
Baokim: It’s not that common. But those individuals with oily skin and sweat a lot are more susceptible since body oils and sweat make the perfect breeding ground. Also those that live in warmer or humid climates have increased risk. Immunocompromised and those on certain medications (like steroids or oral antibiotics) are also predisposed.
 Jenny: Risk factors for fungal acne include:
Jenny: Risk factors for fungal acne include:
- Over use of antibiotic acne
- Heat
- Frequent use of occlusive products
- Often seen in young adults, but can also occur in immunosuppressed individuals
 Mara: It’s not as common as the internet implies it to be. But because of the tropical climate I live in, it might be more common than in temperate regions. Some groups more prone to fungal acne:
Mara: It’s not as common as the internet implies it to be. But because of the tropical climate I live in, it might be more common than in temperate regions. Some groups more prone to fungal acne:
- Adolescents due to increased sebum activity
- Prone to sweating (athletes, overweight, etc)
- Previous use of topical, oral antibiotics, or immunosuppressive agents
- Generally seen more in males
Question #3
Can you distinguish “fungal acne” with your eyes alone?
 Baokim: It can be, to the trained eye! Fungal acne usually presents itself as small, uniform papules and pustules without the presence of comedones (whiteheads or blackheads) or cysts like acne does.
Baokim: It can be, to the trained eye! Fungal acne usually presents itself as small, uniform papules and pustules without the presence of comedones (whiteheads or blackheads) or cysts like acne does.
 Jenny: Often they come as itchy, follicular based papules and pustules and don’t typically respond to traditional acne treatment like topical and oral antibiotics.
Jenny: Often they come as itchy, follicular based papules and pustules and don’t typically respond to traditional acne treatment like topical and oral antibiotics.
 Mara: Usually diagnosis is done based on the patient’s history and physical examination. Occasionally there are cases where further exams are needed because acne and fungal acne affect the sebaceous glands and can have similar appearances.
Mara: Usually diagnosis is done based on the patient’s history and physical examination. Occasionally there are cases where further exams are needed because acne and fungal acne affect the sebaceous glands and can have similar appearances.
Question #4
What are the diagnostic tools commonly used to diagnose “malassezia folliculitis”?
 Baokim: Usually it’s diagnosed based on a patient’s history and clinical appearance. It can be confirmed with KOH wet prep under a microscope, typically doesn’t warrant fungal culture or biopsy but are available to confirm a diagnosis.
Baokim: Usually it’s diagnosed based on a patient’s history and clinical appearance. It can be confirmed with KOH wet prep under a microscope, typically doesn’t warrant fungal culture or biopsy but are available to confirm a diagnosis.
 Jenny: KOH scraping of skin with presence of yeast is diagnostic. More invasive testing includes biopsy.
Jenny: KOH scraping of skin with presence of yeast is diagnostic. More invasive testing includes biopsy.
 Mara: Can be diagnosed with KOH examination or smear where you take a sample of the skin lesion and add a substance then check under a microscope. Can also use a handheld device with black light to examine the lesions with affected areas showing a bright yellow green color. Biopsy and other methods are available as well!
Mara: Can be diagnosed with KOH examination or smear where you take a sample of the skin lesion and add a substance then check under a microscope. Can also use a handheld device with black light to examine the lesions with affected areas showing a bright yellow green color. Biopsy and other methods are available as well!
Question #5
Any treatment options? Skincare you would not recommend for those with “malassezia folliculitis”
 Baokim: Treatment often is a topical or prescription oral antifungal. I recommend checking the table to find what to use and what to avoid.
Baokim: Treatment often is a topical or prescription oral antifungal. I recommend checking the table to find what to use and what to avoid.
| Use | Avoid |
| Ketoconazole (Nizoral shampoo) | Olive oil (skincare) |
| Selenium sulfide (Selsun Blue shampoo) | Coconut oil (skincare) |
| Pyrithione zinc (Head & Shoulders shampoo) | Fatty acids (skincare) |
| Tea tree oil and sulfur helps to maintain (haircare) | Tight clothing |
| Oil free moisturizers (skincare) | Excess sweating |
| Salicylic acid (skincare) | |
| Benzoyl peroxide (skincare) | |
| Retinoids (skincare) |
 Mara: Treatment can be topical antifungals: ketoconazole, clotrimazole, miconazole, etc. However, since topical treatments don’t penetrate well into the hair follicle usually oral antifungals are used and improvements can be seen in 1-2 months. What you can do to keep it under control:
Mara: Treatment can be topical antifungals: ketoconazole, clotrimazole, miconazole, etc. However, since topical treatments don’t penetrate well into the hair follicle usually oral antifungals are used and improvements can be seen in 1-2 months. What you can do to keep it under control:
- Can wax or wane, depends on the weather, humidity, and activity level
- Wear loose clothing when it’s hot and humid
- Change out of clothes immediately after working out or sweating
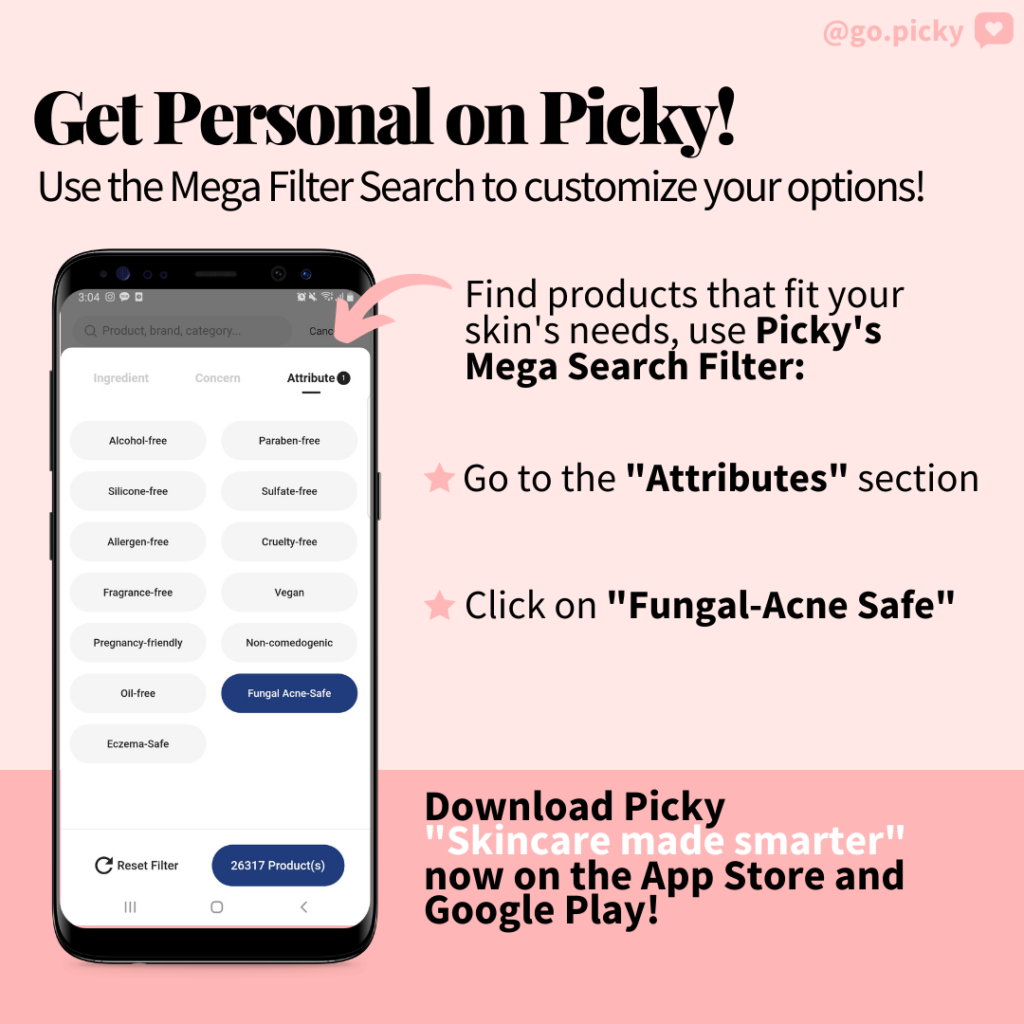
Get Personal on Picky
On Picky, we want you to find exactly what your skin needs! Which is why we have an “Attributes” filter for you to sort through products that are “Fungal-acne safe” among many other concerns such as “Cruelty-free” or “Eczema-safe.” Start using Picky and truly customize your skincare search! Don’t forget to follow us on Instagram and check out more skincare science content on our blog.

















9 Responses
I learned a lot about fungal acne from reading this alone! ♥️
I’ve suffered from fungal acne so long and it’s so hard to get rid of it
Can I get fungal acne from over-moisturizing? I am using a heavy cream as a night cream with sake ferment.
Thank for this info. Actually I’m suffering from this for a years and now I don’t know what to do cuz i can’t go to the hospital to consult my derma…I’m only a 15yr girl and my skin condition starts when I was in grade 6 and time pass by.. and now I can’t handle it anymore I have it on my whole face and I think I have it also on my back😭
internet fooled me 😱😳 now i learn the differences about acne.
Ive been meaning to read this and just never received a chance. Its an issue that Im extremely interested in, I just started reading and Im glad I did. Youre a good blogger, one of the best that Ive seen. This blog certainly has some info on topic that I just wasnt aware of. Thanks for bringing this things to light.
I love when you talk about this type of stuff in your posts. Perhaps could you continue to do this?
Well I truly liked reading it. This post offered by you is very effective for correct planning.
Great article about fungal acne, many mistakes it for regular acne. I also like the form of the article – a discussion between authoritative dermatologists.